JC's Story
July 22, 2025
5
min read
JC was a 9-year-old boy and the youngest child in a family of four, presented with a large swelling on his upper right arm. Medical investigations revealed that JC had late-stage Rhabdomyosarcoma, a rare and aggressive form of cancer. Due to the advanced nature of the disease, the healthcare team provided counseling to both JC and his stepfather before discharging them under total palliative care. However, a follow-up visit two weeks later revealed a complicated family situation. JC and his family were at the chief's house involved in a dispute related to his illness. JC’s mother, who is the second wife, strongly believed that the first wife and her aunt had bewitched her son due to jealousy, highlighting how deeply cultural beliefs were influencing the family’s interpretation of the illness.
Attempts to provide further care were hindered by privacy issues and the family's movements. On a subsequent visit, the healthcare team found did not find the patient and guardian at home and were informed that they had gone for prayers. However, there was suspicion that they had visited a herbalist. During the next home visit, JC was found to be in severe pain and the swelling on his arm had ruptured. The healthcare team provided pain management and wound care and also conducted a family meeting to offer end-of-life counseling. It was during this session that JC’s mother disclosed suicidal thoughts, calling for immediate psychosocial support and counseling. Unfortunately, four days later, JC passed away. The healthcare team conducted a bereavement visit after 2 weeks.
This case highlights significant gaps in the healthcare system regarding children’s palliative care. One of the major challenges is the lack of continuity in care, especially at lower-level health centers. There are insufficient resources, including trained personnel and logistical support such as transportation which are critical in delivering comprehensive and consistent palliative care services. These limitations hinder timely follow-ups, home visits and the ability to monitor the psychosocial wellbeing of both patients and their families. Furthermore, there is a lack of structured systems to address cultural beliefs and family dynamics which can significantly affect the care process.
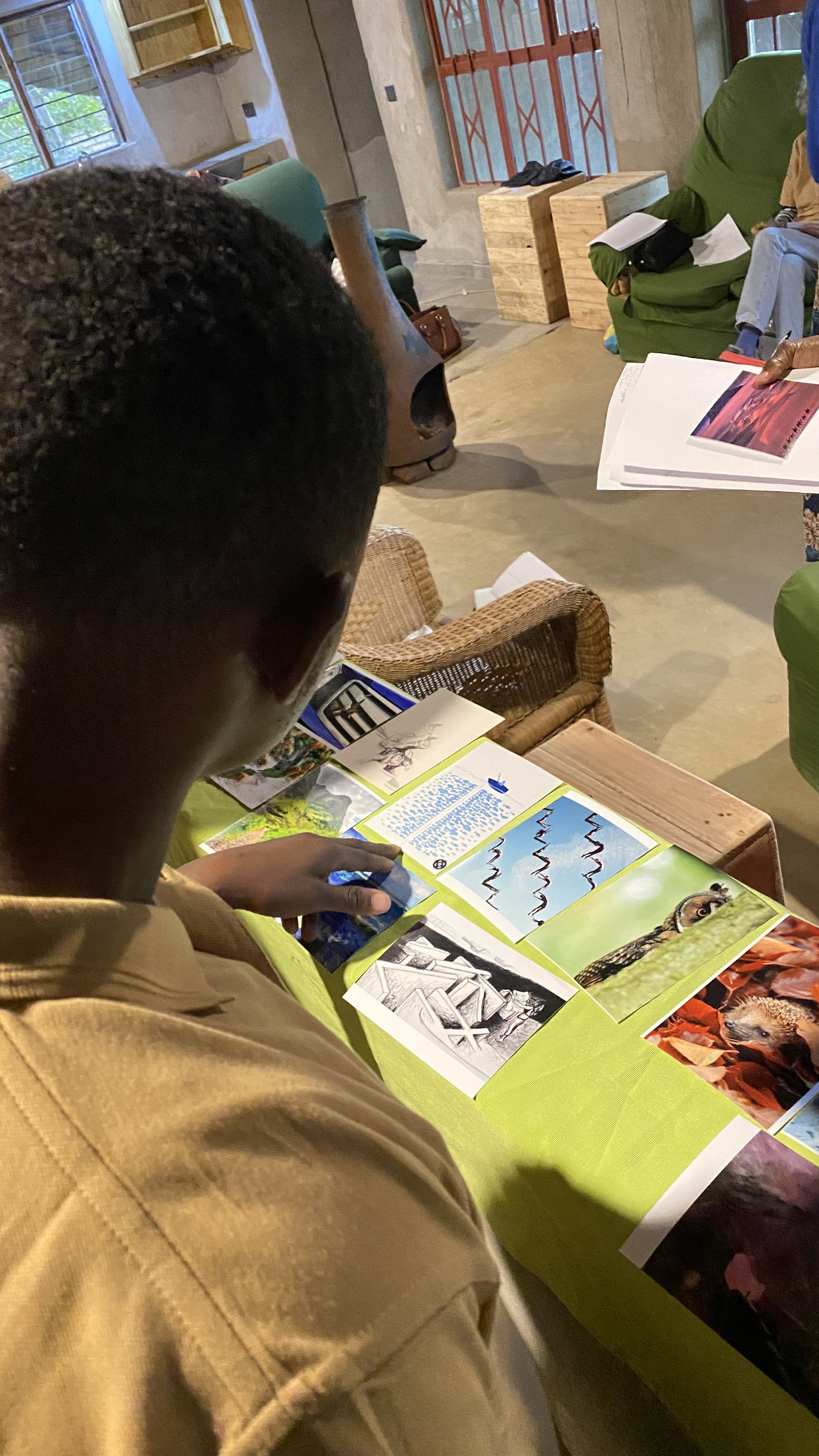
Below are pictures taken with consent during our last home visit.
NB: Viewer disclaimer


Key Lessons
1. Cultural Beliefs and Family Conflicts: Even with appropriate medical and palliative care, cultural beliefs and family disputes can hinder effective care.
2. Importance of Consistent Follow-up: Regular follow-up visits are essential in palliative care as they help healthcare providers understand the evolving needs of both the patient and family.
3. Need for Advocacy and System Integration: There is a pressing need to advocate for children’s palliative care across all levels of the healthcare system.
This includes:
· Training healthcare workers in palliative care.
· Establishing community outreach programs.
Educating families to reduce stigma and correct cultural misconceptions.
National Bank Accounts