SS' Story
July 22, 2025
5
min read
SS is a 5-year-old girl who was diagnosed with Neuroblastoma towards the end of 2024. She is the only child of a 22-year-old single mother who has been her main caregiver since diagnosis. The family lives in a low-resource setting with minimal social support. Following a period of active treatment, the medical team determined that curative treatments were no longer possible and the child was discharged from the hospital for total palliation. She was referred to the Palliative Care Team in May 2025 for support with symptom management and emotional counseling.
Three weeks after discharge, the Palliative Care Team conducted a home visit to follow up on the child's condition and to assess the family’s needs more comprehensively. During the home visit, a holistic assessment was done focusing on the physical, psychological, social and spiritual dimensions of care.
Physically, SS was experiencing moderate pain, but this was well managed with oral liquid morphine which the mother was administering appropriately. However, the team noted that SS had developed new symptomsincluding headache, ataxia (loss of coordination or balance) and blurred vision. These symptoms are clinical indicators of disease progression, likely reflecting central nervous system involvement of the neuroblastoma. This was deeply concerning as it showed a shift in her clinical condition that required further adjustment in care and anticipatory planning. The Palliative care team therefore provided the patient with Paracetamol to help controlling the headache.
Psychologically, during the counseling session, the child’s mother became visibly distressed and eventually broke down emotionally. She expressed feelings of overwhelm, helplessness and anticipatory grief. At only 22 years old, she is facing the huge emotional burden of caring for a terminally ill child entirely on her own. Her reaction reflected both the emotional pain of seeing her child’s condition worsen and the mental exhaustion from prolonged caregiving without a support system.
Socially, the family was found to be living in socially vulnerable conditions. They had no consistent income and the mother had to give up work to care for her child full-time. The lack of extended family support or community resources left them isolated. Recognizing this, the palliative care team took steps to provide psychosocial support and nutritional support (Likuni phala, Maize flour, Soya pieces, Milk, Cooking oil) and Vaseline.
Spiritually, the visit was supported by the presence of the part-time chaplain, who played a significant role in addressing the mother’s spiritual needs. The mother shared that she believes in God and prays often. At her request, the chaplain led a brief prayer session which brought her a sense of comfort and peace. This moment was deeply moving for both the mother and the care team. It highlighted how spiritual care can provide strength, meaning and hope especially in times of deep emotional pain.
This case is particularly heart breaking and complex. It brings out the emotional depth of pediatric palliative care, especially when the primary caregiver is young, alone and unsupported. The scenario not only highlights the child’s suffering, but also the emotional, psychological impact the illness has on her mother.
From a care perspective, the case is a powerful reminder that palliative care extends beyond symptom controlas it also involves emotional and psychosocial care for the caregivers who are often the invisible patients. For the palliative care team, this case showed a deep sense of empathy and emotional connection, and it challenged us to go beyond our routine interventions to creatively and compassionately support both mother and child.
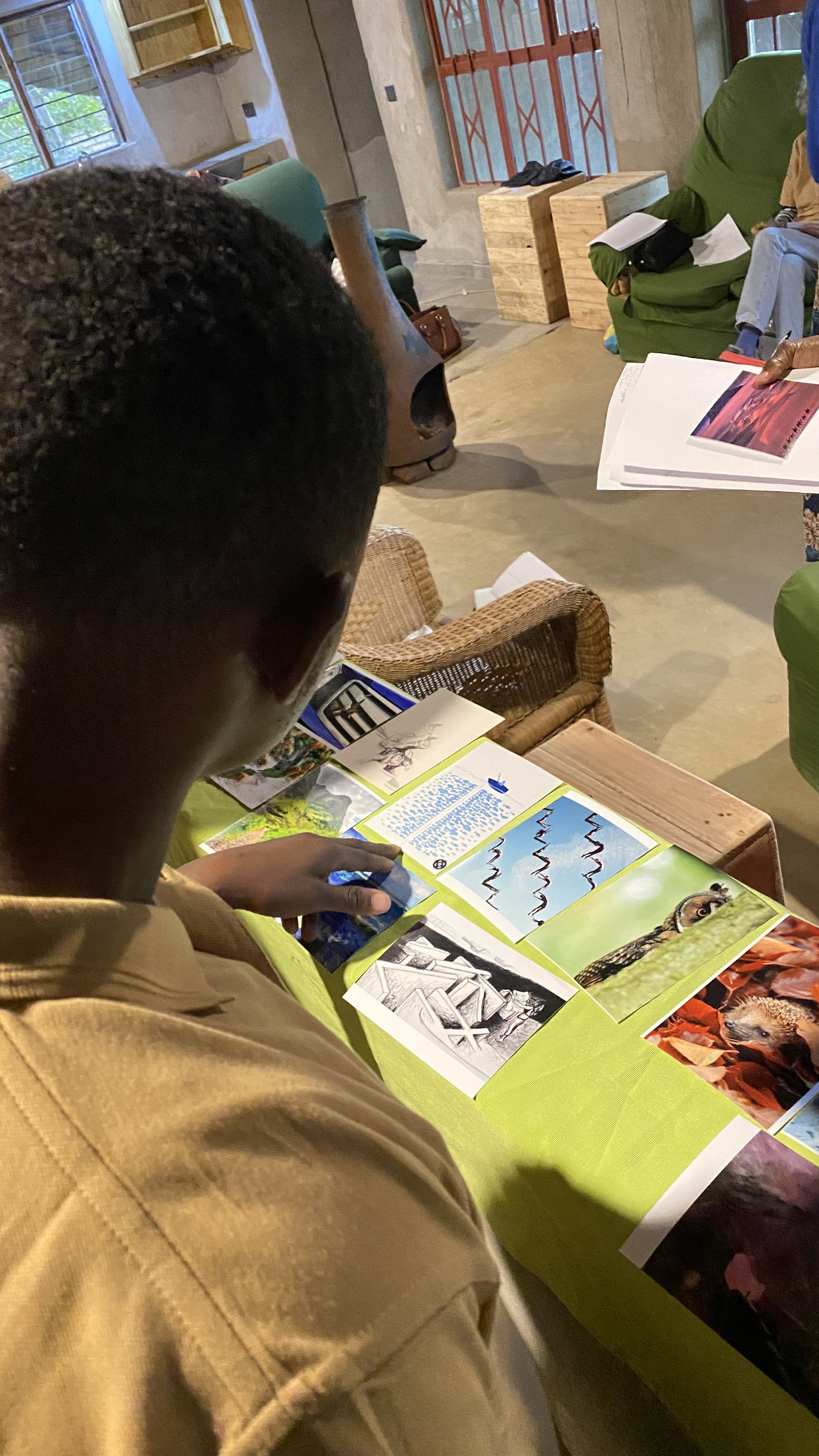
Below are pictures taken with consent during the home visit.




National Bank Accounts